I think these are valid concerns, once again, and must be discussed and hashed out so that everyone is on the same page.
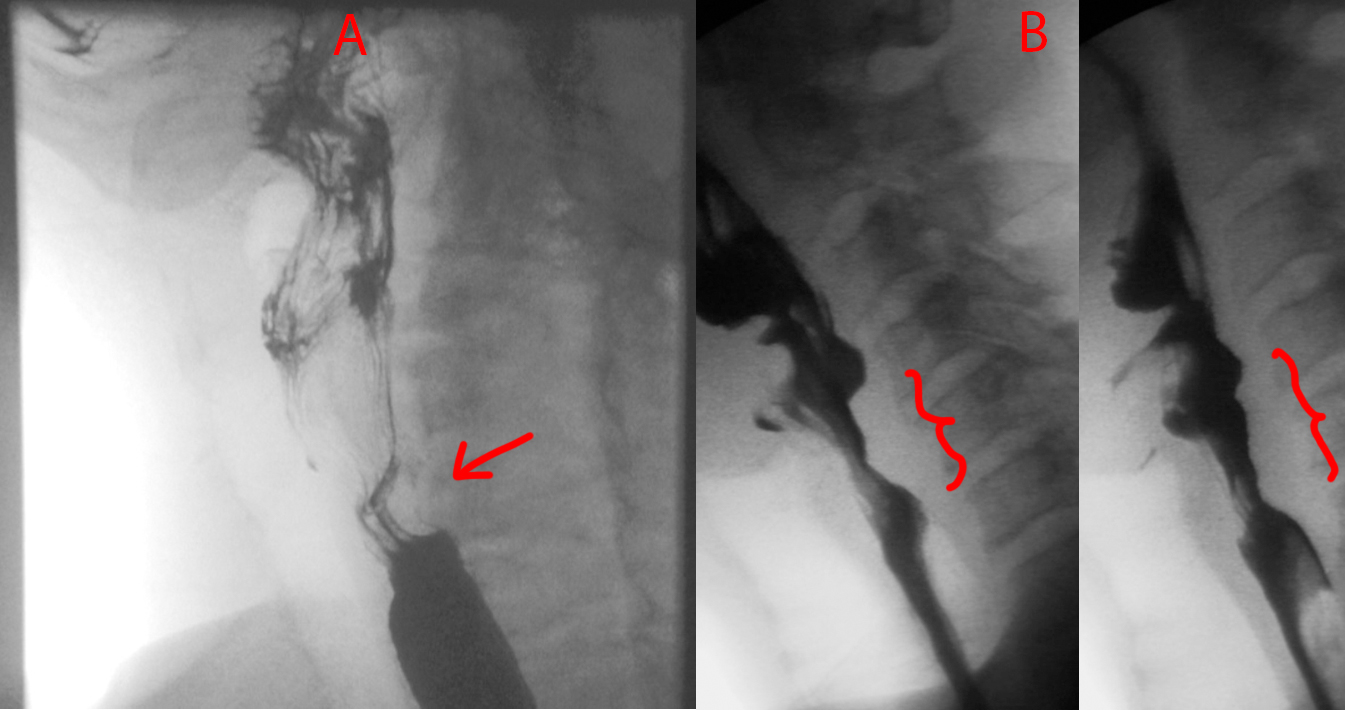
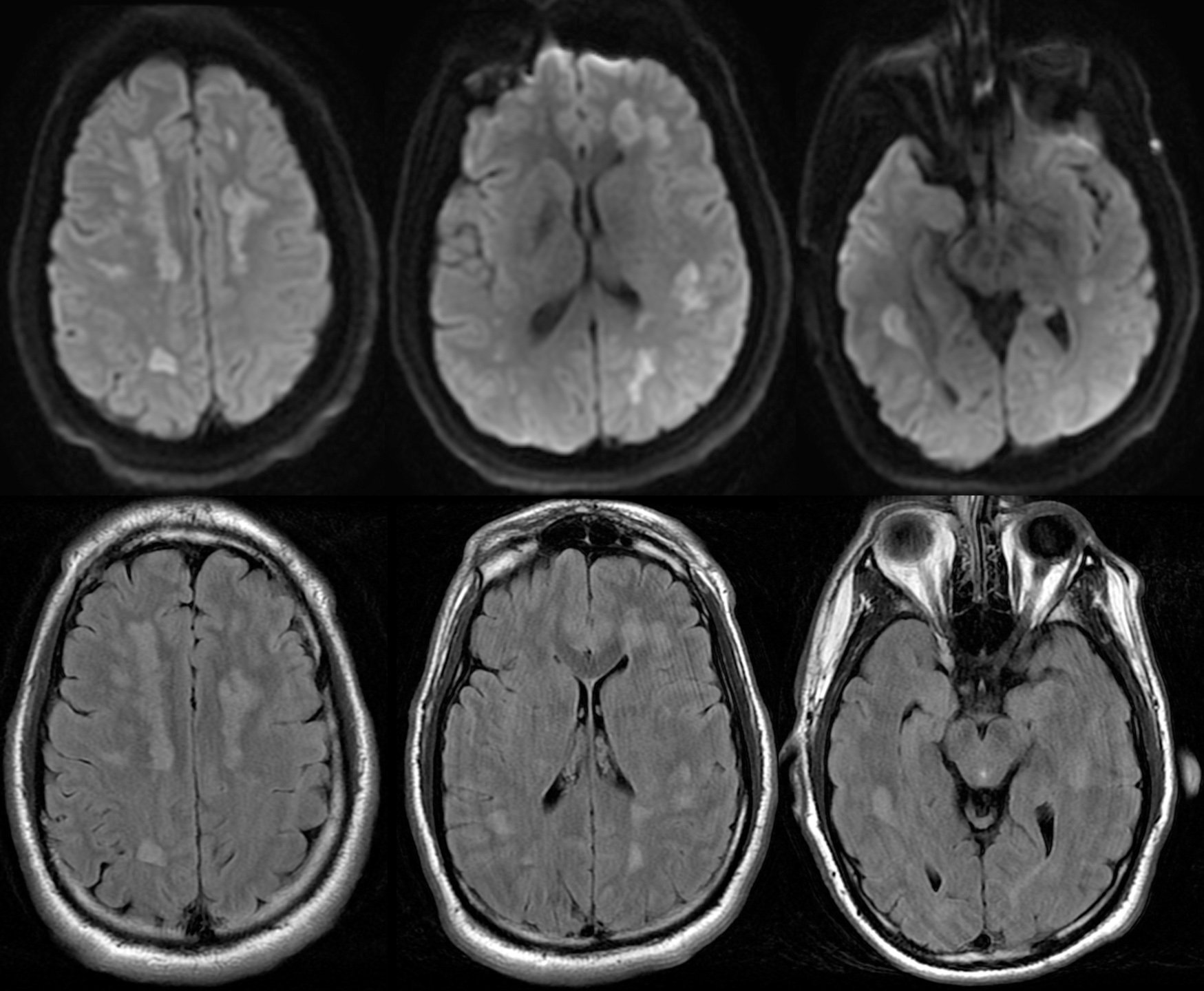
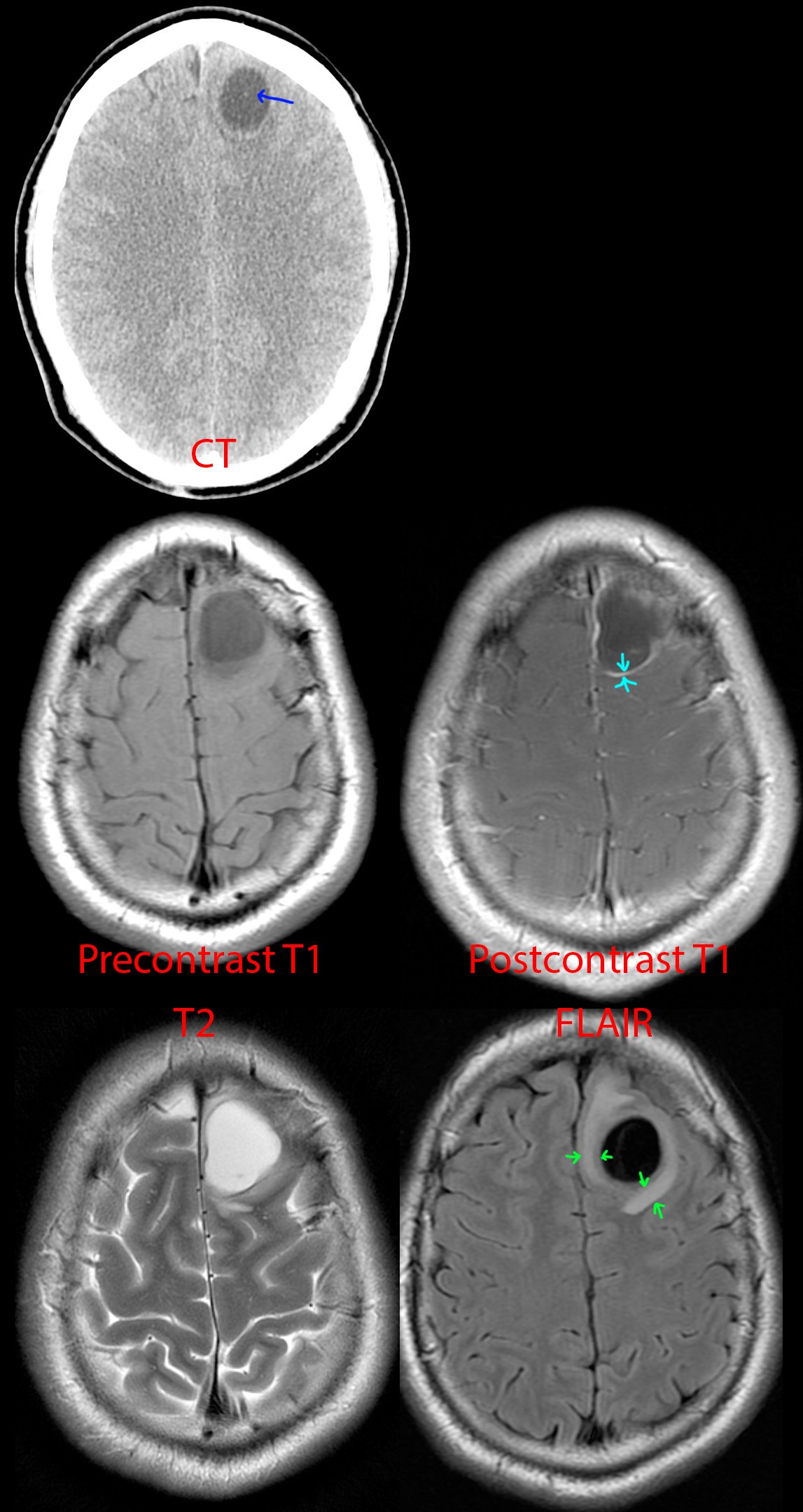
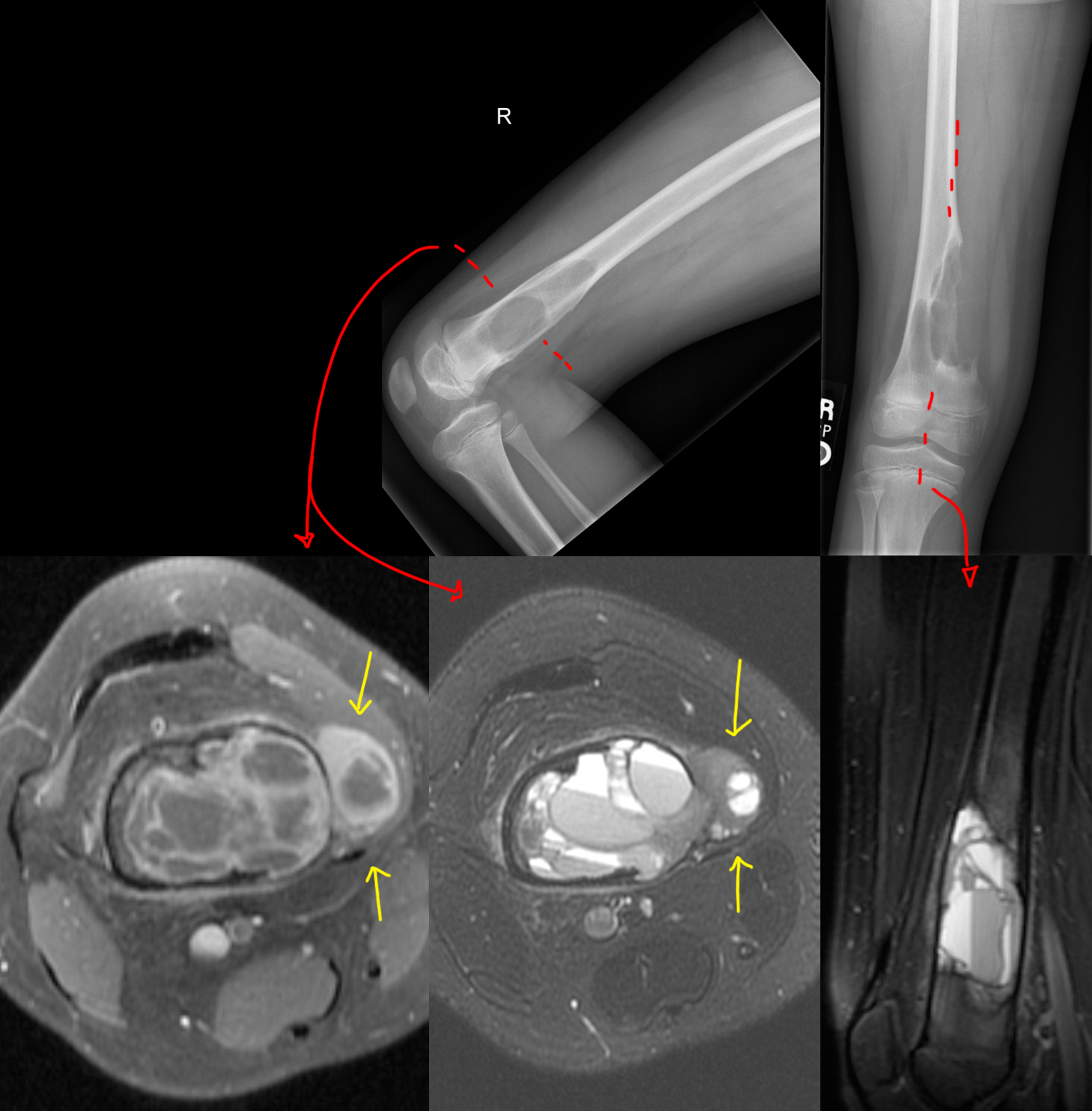
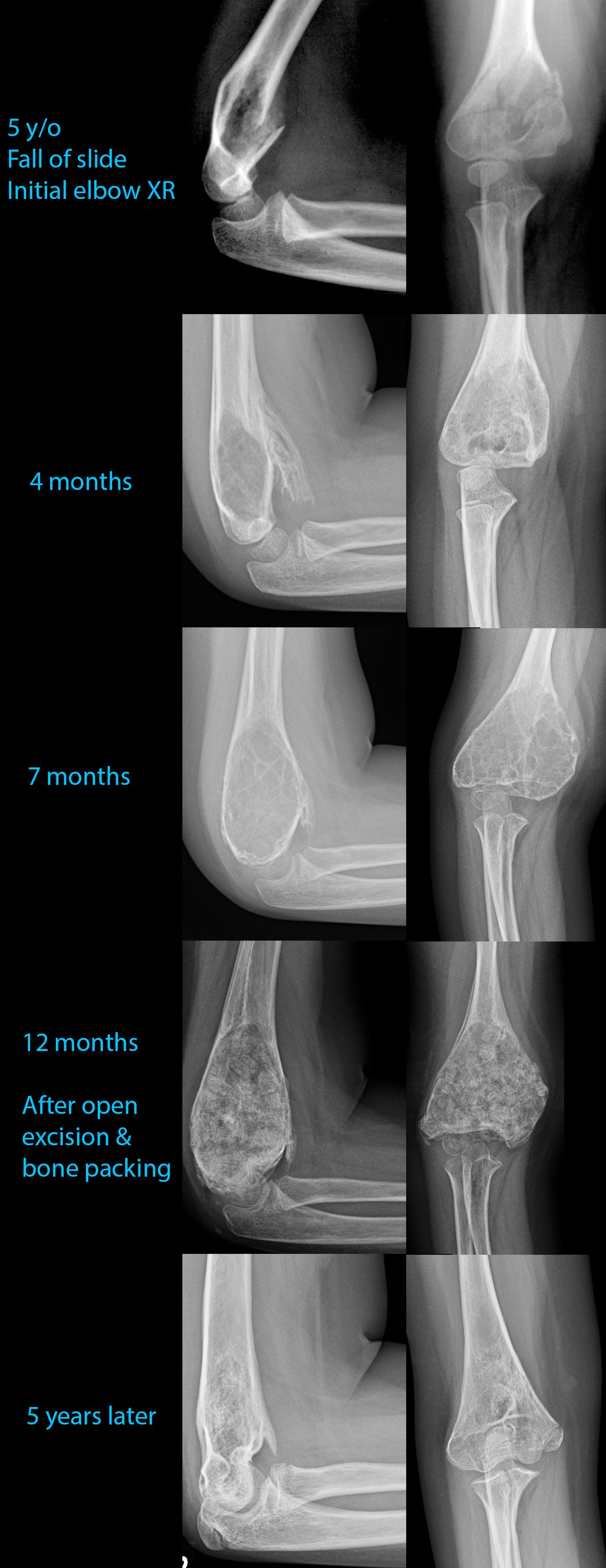
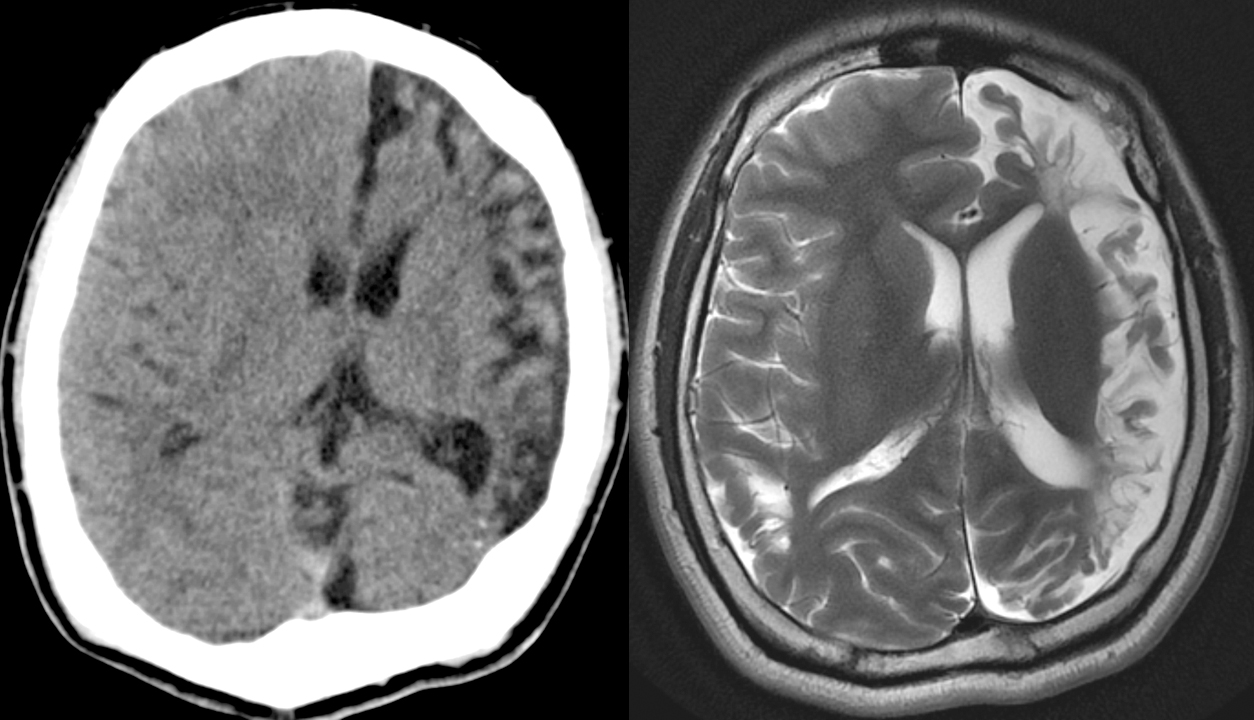
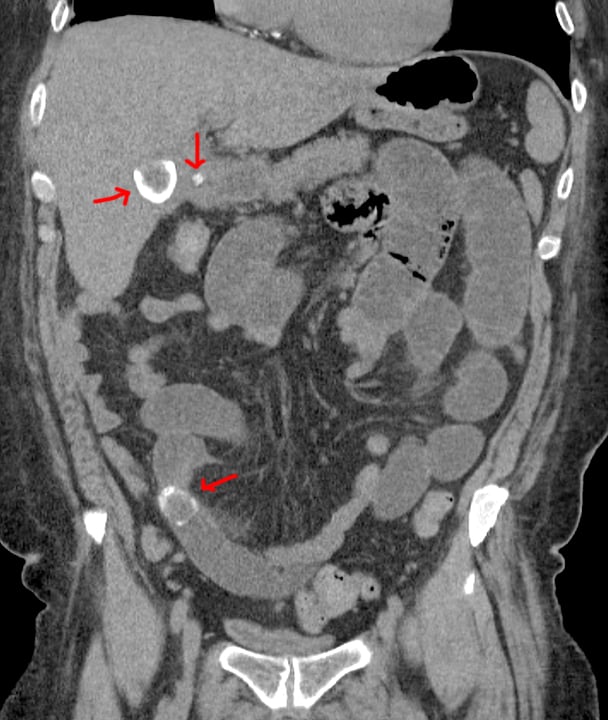
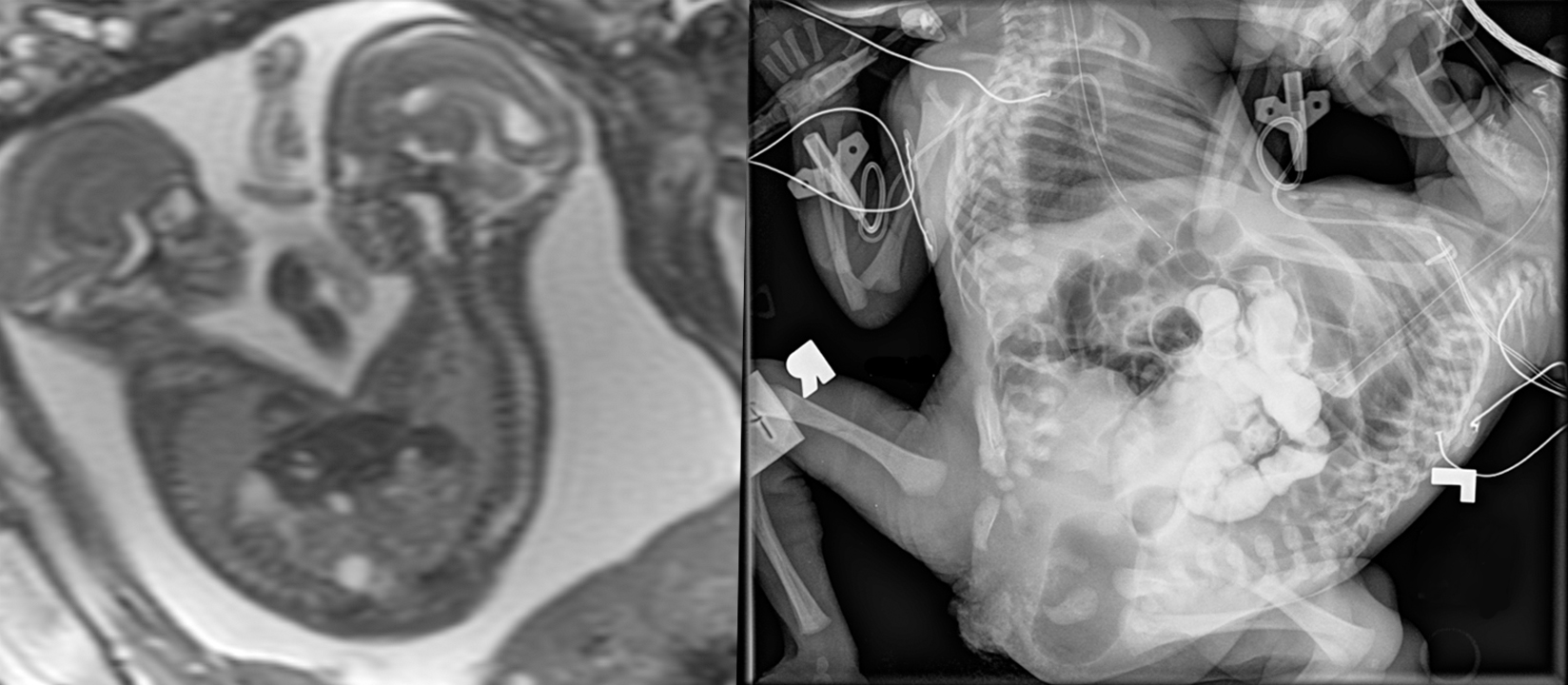
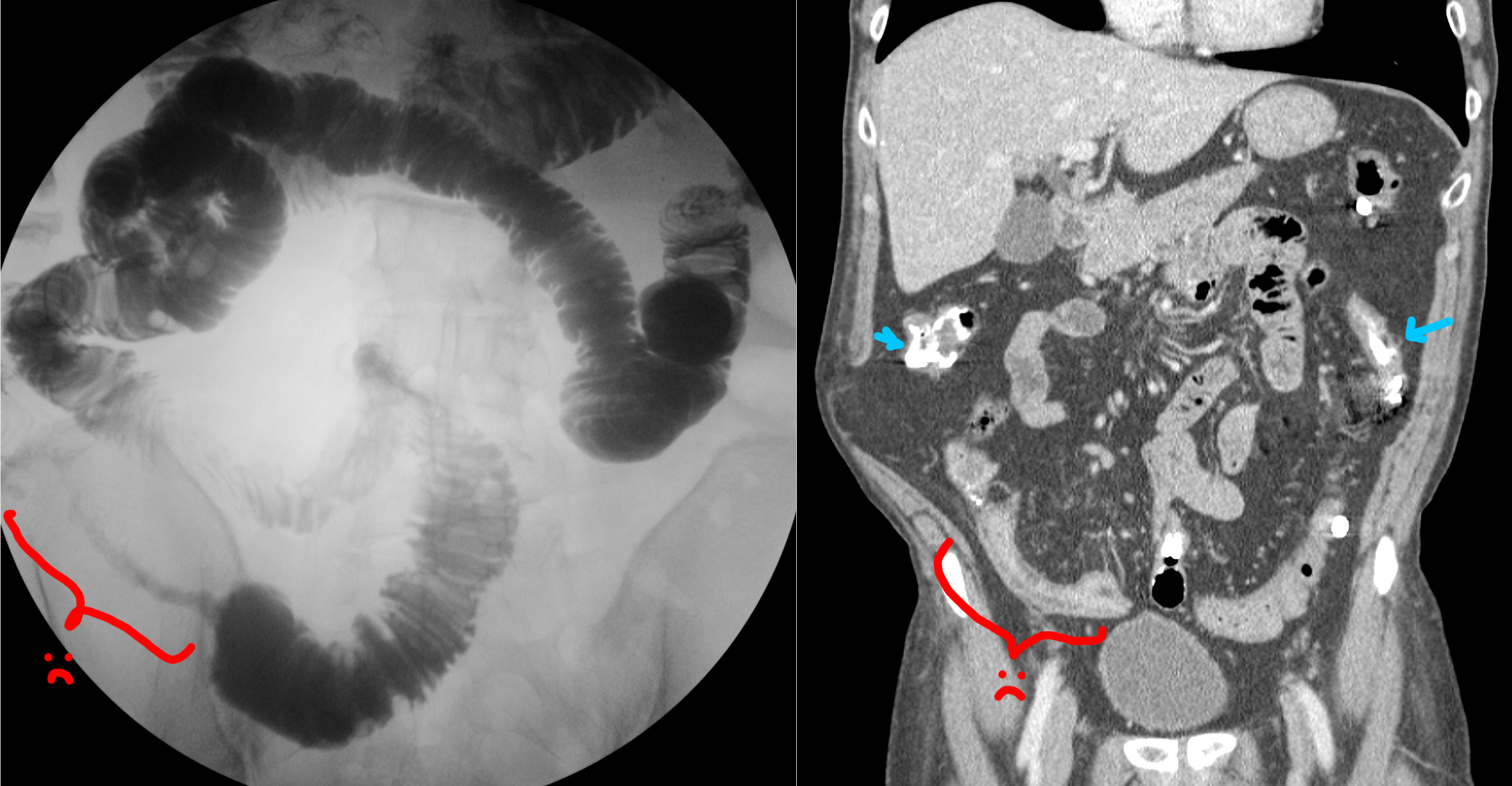
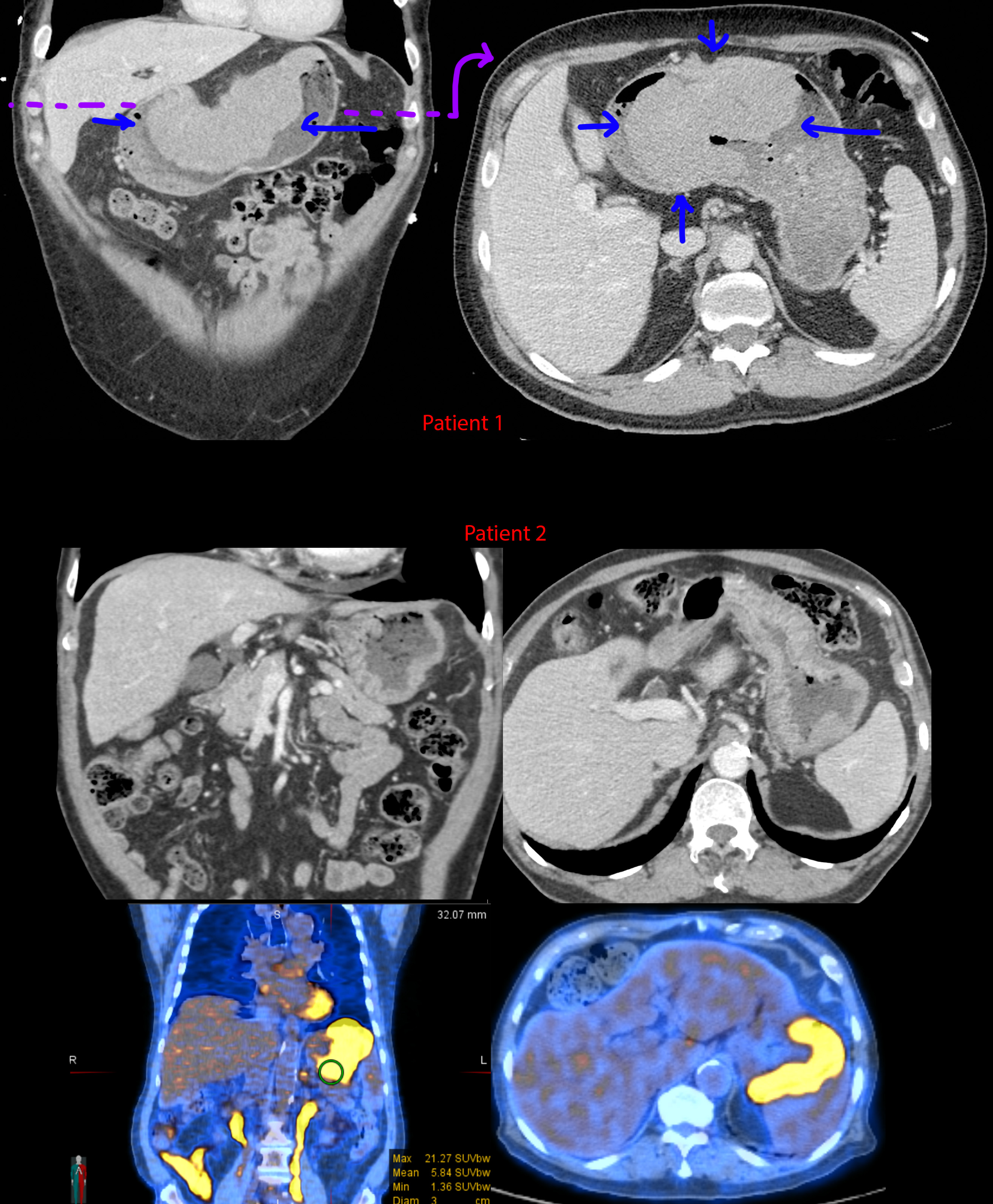
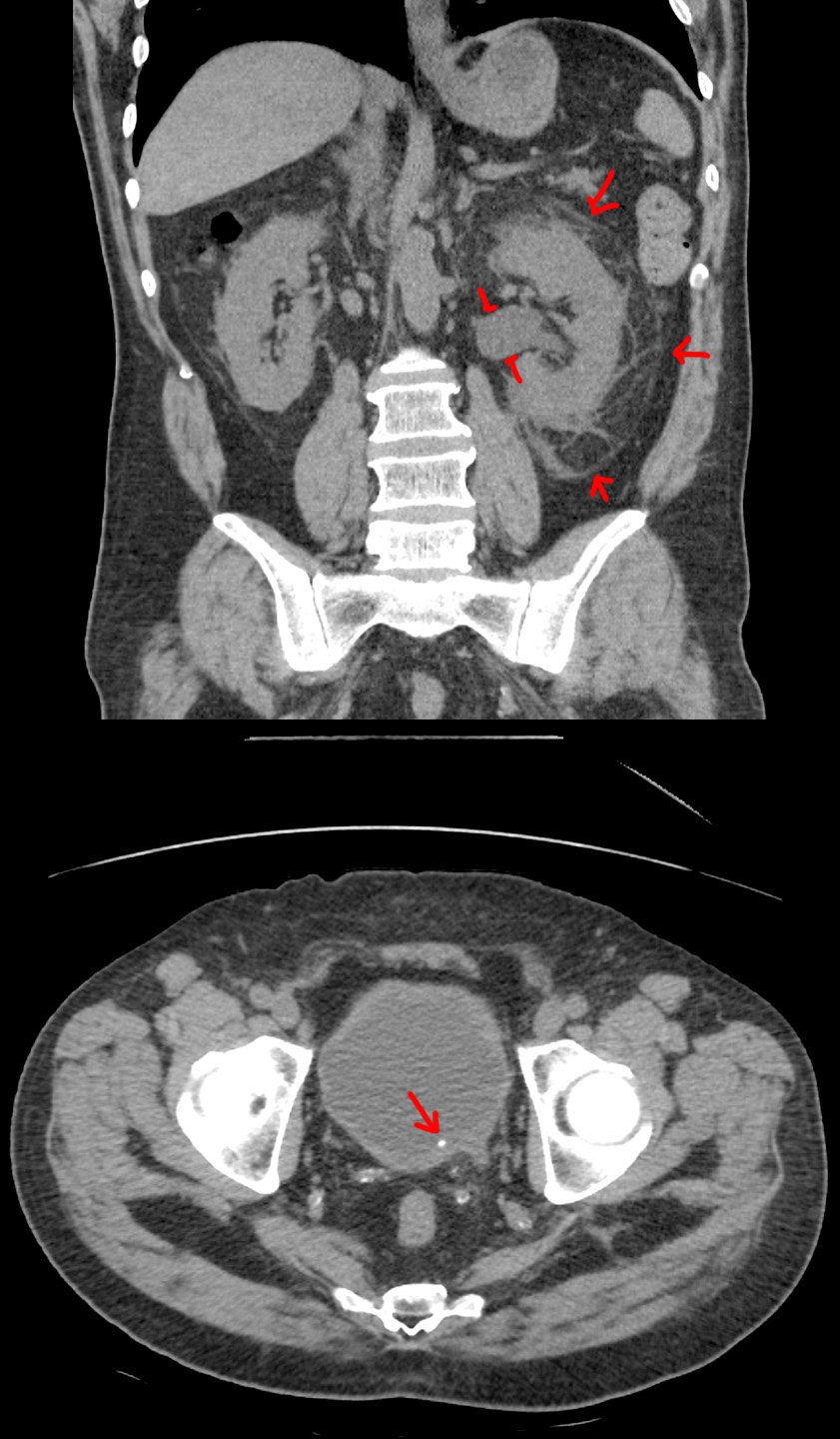
The medical field has a long history of sharing cases for education, and I would say radiology definitely is one of the fields where this is done more often than not, due to the complexity of cases, use of imaging, which is a format that makes it easier to share. I would also say that radiology is quicker to embrace new technologies, including use of the internet and social media, due to reliance on technology to begin with. For example, you can find on twitter, of all places, many case presentations and discussions, many by prominent leaders in the field. Almost all the major radiology societies have some case series for perusal, there’s Radiopaedia as I already mentioned, and the largest community I’m aware of is r/radiology, which I modeled this community after.
I understand there’s a slippery slope between posting educational content and entertainment content. I intend to firmly keep us away from the entertainment side. While I do not want this community to fall into a somber tone, I will not tolerate posts or comments intended to mock or demean a case/patient.
In regards to data harvesting - interesting thought. I had to dig a little bit. There’s definitely been some publications that deal with large medical imaging datasets wherein AI was able to use the high resolution imaging to identify patient features, including 3D reconstruction of the face from the data. The images posted here are: 1) regular .jpgs and not high resolution files like dicom, 2) limited to a couple of images when a full CT can be in the hundreds, and 3) been through photoshop, powerpoint, possibly multiple saves though jpg with degradation each time, or they’re crappy phone camera images of a medical image. I can’t say the risk is absolutely 0, but it’s pretty close - by staying within medical privacy laws and avoiding super rare presentations of things.
However, your concerns have been my concerns too, so I have also reached out to the .world admins for their thoughts. Perhaps they don’t feel comfortable hosting this type of content, or would like to see some other assurances. I will find out and proceed from there.

Should the instances that responded to you be refederrated? I’m pretty sure I saw some of them on lemmy.world’s block list. I think it would be sad for these small servers to not realize they are, in fact, not connected to the greater fediverse. On the other hand, if you’re an admin, and you don’t know what you’re doing to the point of not knowing your server was infected by hundreds of thousands of bots, maybe it’s too dangerous to refed.