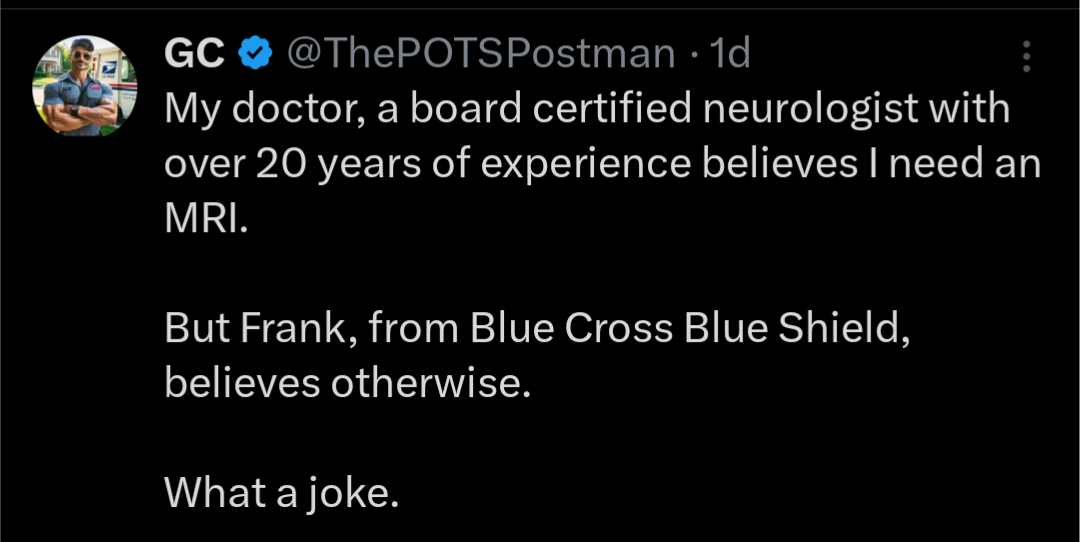
No way ? insurances have a say against the word of doctors ? I must be hallucinating, I thought I knew all about it
Microblog Memes
A place to share screenshots of Microblog posts, whether from Mastodon, tumblr, ~~Twitter~~ X, KBin, Threads or elsewhere.
Created as an evolution of White People Twitter and other tweet-capture subreddits.
Rules:
- Please put at least one word relevant to the post in the post title.
- Be nice.
- No advertising, brand promotion or guerilla marketing.
- Posters are encouraged to link to the toot or tweet etc in the description of posts.
Related communities:
Well. No. They have a say about whether they'll pay for what the doctor has decided is best for the patient.
Everyone should also remember that it's going to get worse. People, especially nurses, are leaving the medical field. GPs are becoming scarce, and boomers are taking more and more of the medical resources available as they age. It's going to get harder and harder to get timely medical care at all, let alone getting it without bankruptcy.
I really believe a lot of this comes down to poorly automated systems and people not allowed to go off script … and insurers have no reason to change this.
When there’s a claim it gets entered into the insurer system by procedure code. It’s only decided based on what procedure code is recognized by the system. The peon deciding to reject it likely has no power to say otherwise nor incentive to. Even when they do ask for a doctors opinion, do you really think he reads all the case notes, or even has access to them, or has time to read them, or incentive? Nope, just whatever codes were entered into the system. You read a lot about issues where procedures have to be recoded for insurance, but I’ll bet many more of the rejects are as simple as the code not supporting the treatment and no one at the insurer looking farther. This is more a form of institutional incompetence but insurers have a profit motive in maintaining this incompetence
I did pharmacy billing for a while and this is a kind of innocent take that people are just being lazy. The training was terrible (I was taught the basics of the software and then given a photocopy of various employees hand written notes for common rejection solutions over the years ....most of which didn't still apply and those employees had long left; when I left in sure my notes were copied to the pile). There were metrics that kept being increased meaning spending more than 30 seconds on a claim was going to put you behind (I did night shift and my boss was talked to about me once or twice because I sometimes had an hour or two where I'd cleared everything I could and had nothing to do because the rest of the world was asleep). And, finally:
The software was designed to actively fight us. My most common reject was insurance won't pay for anything $X or more with X being stupidly low. For many insurances you could not put in a recurring override for monthly maintenance meds. Your options were either give the patient a 2/3/whatever day supply to get the cost down and they'd just have to visit the pharmacy for pickup so much they might as well work there. Or do a one time special override every. Single. Time. Which involved me doing a special code on my end (which wasn't the same for every insurer and sometimes they'd just randomly change it for shits and giggles with no communication, I had a list of codes that were often used I'd try guessing with). Calling their help desk whose employee retention and training were also in the toilet. If the insurance end person knew the process for a one time special override, great. If not I started specifically keeping notes by insurer to teach new people because otherwise I'd be subjected to an hour of phone hockey while they tried to find someone who both knew how to do it and could cram my call into their metrics. Then we'd have to go through generating specific rejects just because we needed it in our logs we tried shit we knew wasn't going to work. Doctor note saying md knows med is expensive and that pt needs it to live regardless attached? Okay run it through as cost doctor approved to get the "fuck the doctor we don't want to pay" reject. Insurance doctor/nurse team reviewed that yes the doctor is correct the patient needs this med to live code put in? Okay run it again to get the fuck our own doctors we still won't pay reject. Now insurance help desk has to message their next level support to get authorization for a one time override for medical necessity. Okay now it'll go through on the insurer end (as long as they didn't fatfinger anything because the override only works for one single attempt). Great, we did it one try team! Now my turn to do it on my end which involves me removing all my codes because the software no longer recognizes the reject so will reject me for needless codes which will make us have to get the One Single Try Authorization again......
You don't have to die to visit hell just work in medical billing.
What a graphic presentation of life in hell
Think we could make Lemmy a household name by having the C suite of companies that do this SWATed? The government doesn't work so we're going to have to do this ourselves.